
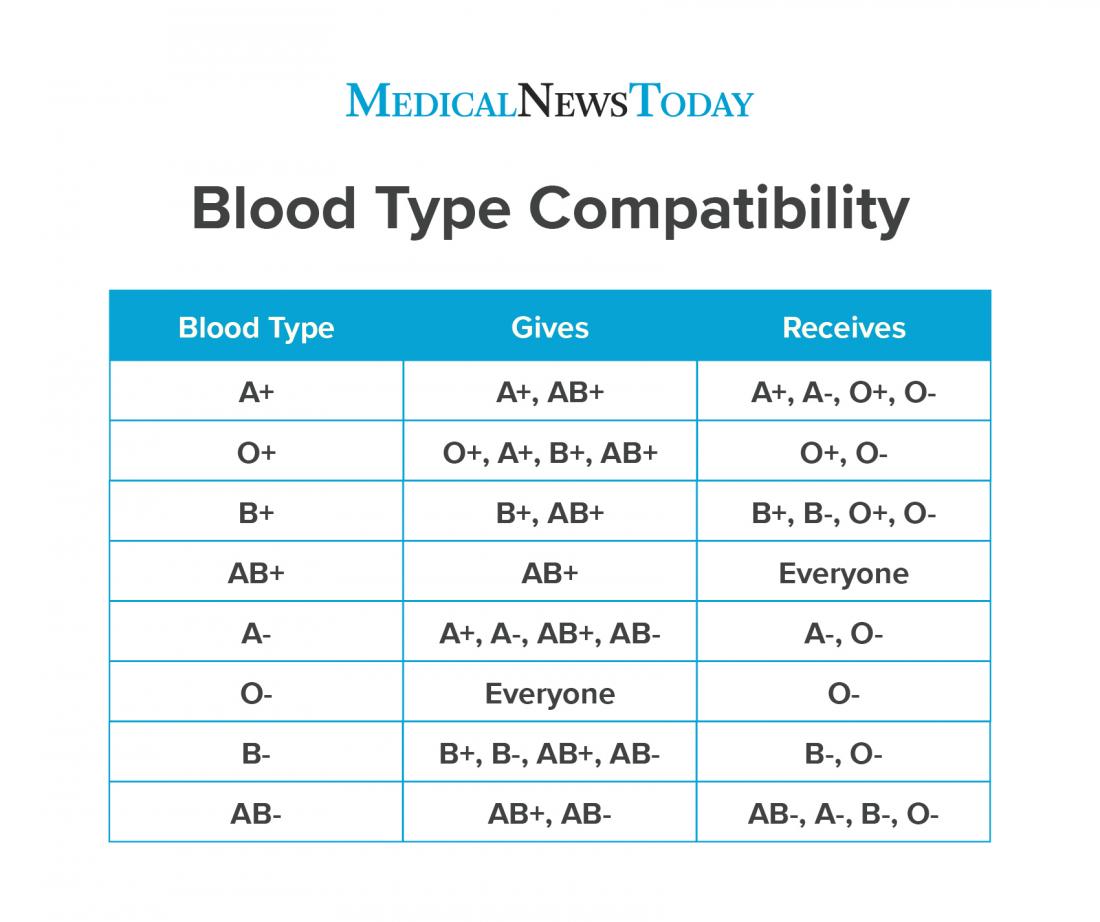
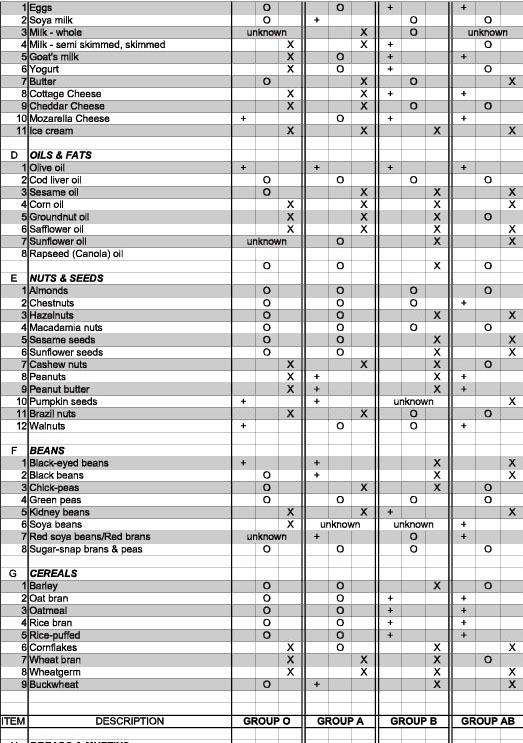
How is Alloimmunization diagnosed?Īll mothers are tested for the development of antibodies three times during pregnancy: at their first prenatal visit, at 28 weeks’ gestation, and at delivery. However, once the antibodies have formed, your body does not get rid of them, so any subsequent babies are more likely to have problems if they have the same blood type as the first baby. If hemolytic disease is left untreated it may lead to serious problems, such as brain damage hydrops fetalis (**LINK**) (abnormal amounts of fluid build-up in two or more body areas) seizures problems with mental function, movement, hearing and speech, or even death.Īlloimmunization does not usually cause problems during a first pregnancy because the baby often is born before many of the antibodies develop. Without enough red blood cells, your baby won’t get enough oxygen. This is called hemolytic disease of the fetus, a condition in which red blood cells are destroyed faster than the body can replace them. Those antibodies can cross back through the placenta and attack your baby’s red blood cells. If your blood type is different than your baby’s, your immune system may treat the baby’s blood cells as if they were a foreign substance and produce antibodies against them. During pregnancy, red blood cells from your unborn baby can cross into your bloodstream through the placenta. It is a condition that may occur during pregnancy when there is an incompatibility between your blood type and your baby’s blood type. Read more about treating rhesus disease and the potential complications of rhesus disease.Alloimmunization, often called Rh-isoimmunization or Rh incompatibility was first described in Rh negative women with an Rh-positive fetus, but it can occur with many other blood type incompatibilities. However, treatment is usually effective and these problems are uncommon. In other cases, it could lead to brain damage, learning difficulties, hearing loss and blindness and vision loss. If rhesus disease is left untreated, severe cases can lead to stillbirth. Treatment for rhesus disease after delivery can include a light treatment called phototherapy, blood transfusions, and an injection of a solution of antibodies (intravenous immunoglobulin) to prevent red blood cells being destroyed. After delivery, the child is likely to be admitted to a neonatal unit (a hospital unit that specialises in caring for newborn babies). A blood transfusion to the unborn baby may be needed in more severe cases. If an unborn baby does develop rhesus disease, treatment depends on how severe it is.
Read more about preventing rhesus disease and diagnosing rhesus disease. The pregnancy will be monitored more closely than usual, as will the baby after delivery. If a woman has developed anti-D antibodies in a previous pregnancy (she's already sensitised) then these immunoglobulin injections don't help. This anti-D immunoglobulin helps to remove the RhD foetal blood cells before they can cause sensitisation. If the mother is RhD negative, she'll be offered injections of anti-D immunoglobulin at certain points in her pregnancy when she may be exposed to the baby's red blood cells.
Rhesus disease is uncommon these days because it can usually be prevented using injections of a medication called anti-D immunoglobulin.Īll women are offered blood tests as part of their antenatal checks and tests to determine whether their blood is RhD negative or positive. Read more about the causes of rhesus disease. The antibodies can continue attacking the baby's red blood cells for a few months after birth. If she's pregnant with an RhD positive baby, the antibodies can cross the placenta, causing rhesus disease in the unborn baby. If sensitisation occurs, the next time the woman is exposed to RhD positive blood, her body produces antibodies immediately. Sensitisation happens when a woman with RhD negative blood is exposed to RhD positive blood, usually during a previous pregnancy with an RhD positive baby. The woman’s body responds to the RhD positive blood by producing antibodies (infection-fighting molecules) that recognise the foreign blood cells and destroy them. The mother must have also been previously sensitised to RhD positive blood.
Rhesus disease only happens when the mother has rhesus negative blood (RhD negative) and the baby in her womb has rhesus positive blood (RhD positive). Read about the symptoms of rhesus disease in a baby. Rhesus disease doesn't harm the mother, but it can cause the baby to become anaemic and develop newborn jaundice. It's also known as haemolytic disease of the foetus and newborn (HDFN). Rhesus disease is a condition where antibodies in a pregnant woman's blood destroy her baby's blood cells.


 0 kommentar(er)
0 kommentar(er)
